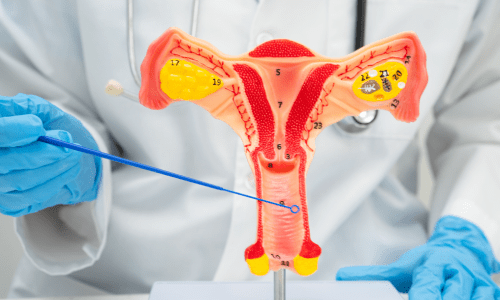
Understanding Vaginal Surgeries
Vaginal surgeries include reconstructive and aesthetic options tailored to individual needs. Common types involve repairing or tightening tissues affected by childbirth, aging, injury, or congenital conditions. These procedures fall under gynecology and increasingly under cosmetic gynecology, where the focus may include improving aesthetics alongside functionality.
Common Types of Vaginal Procedures
Several well-established vaginal surgeries cater to specific goals:
- Vaginoplasty (often called vaginal tightening or rejuvenation) repairs or narrows the vaginal canal. It tightens stretched muscles and removes excess tissue, commonly sought after multiple vaginal deliveries or due to natural laxity over time. This can improve sensation during intimacy and address issues like mild urinary incontinence.
- Labiaplasty reduces or reshapes the labia minora (inner lips) or majora (outer lips). Women may choose this to relieve physical irritation from clothing, exercise, or intercourse, or to achieve symmetry and a preferred appearance.
- Hymenoplasty reconstructs the hymen, typically for cultural, personal, or psychological reasons. It involves repairing or recreating the thin membrane at the vaginal opening.
- Other related procedures include perineoplasty (tightening the perineal area) and clitoral hood reduction, often combined for comprehensive results.
These surgeries can be performed surgically under anesthesia, with some non-surgical alternatives like laser treatments available for milder cases.
Benefits and Considerations
Many women report significant improvements in quality of life after these procedures. Benefits often include enhanced sexual satisfaction, reduced pain or discomfort during daily activities, boosted self-esteem and better hygiene or clothing fit. For reconstructive cases, such as post-trauma or prolapse-related repairs, the primary goal is restoring normal function and comfort.
However, like any surgical intervention, vaginal procedures carry potential risks. These may include infection, bleeding, scarring, changes in sensation, prolonged healing or dissatisfaction with results. Recovery typically involves rest, avoiding strenuous activity or intercourse for several weeks and following post-operative care to minimize complications. Outcomes vary based on individual anatomy, surgeon expertise and realistic expectations.
Important Advice
Vaginal surgeries should always involve thorough consultation with a qualified gynecologist or specialist in cosmetic gynecology. A detailed discussion covers motivations, expected results, alternatives (such as pelvic floor exercises or non-invasive therapies), and evidence-based information. Organizations emphasize informed consent, noting that purely cosmetic procedures lack extensive long-term data in some cases.
Women considering these options deserve compassionate, evidence-based care to make empowered decisions about their bodies.
