What is Hysteroscopy and Why is it Performed?
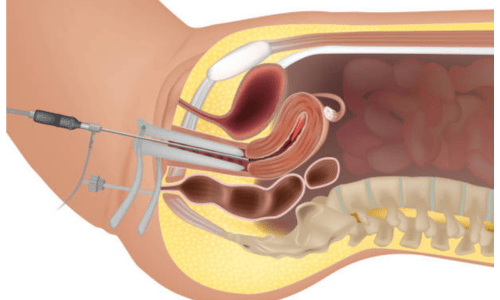
Hysteroscopy serves dual purposes: diagnostic and operative. In its diagnostic form, it helps identify the root causes of abnormal uterine bleeding, recurrent miscarriages, infertility challenges, or unexplained pelvic pain. Common findings include uterine polyps, submucosal fibroids, intrauterine adhesions (scar tissue), or congenital abnormalities. When performed operatively—often called hysteroscopic surgery—the same tool enables real-time interventions. Specialists can remove polyps or small fibroids, resect adhesions to restore normal uterine shape, take targeted biopsies for further testing, or even address issues like retained products after pregnancy. This one-step process avoids the risks and extended downtime associated with traditional open surgery.
The procedure is typically done on an outpatient basis, often in a clinic or hospital setting. Depending on complexity, it may use local anesthesia, sedation, or general anesthesia for comfort. A fluid (saline or similar) is introduced to gently expand the uterus for clear viewing. Most women report only mild cramping during or after the procedure, similar to menstrual discomfort.
Benefits and Recovery
One of the greatest advantages of hysteroscopy is its minimally invasive nature. Patients experience shorter recovery times—many resume normal activities within a day or two—compared to conventional surgery. It offers high accuracy in diagnosis, reduces the need for more invasive procedures, preserves fertility in cases involving polyps or fibroids, and lowers complication rates such as infection or excessive bleeding. For women dealing with heavy periods, infertility, or structural uterine issues, hysteroscopy provides effective relief with quicker return to daily life.
Recovery is generally straightforward. Mild spotting, cramping, or discharge may occur for a few days, managed with over-the-counter pain relief. Patients are advised to avoid tampons, intercourse, or strenuous activity for about one to two weeks to minimize infection risk. Serious complications, like uterine perforation or fluid overload, are rare when performed by experienced specialists.
In expert hands, such as those of qualified gynecologists specializing in women’s health and minimally invasive techniques, hysteroscopy stands out as a safe, efficient solution for uterine concerns. It empowers women with accurate answers and targeted treatments, promoting better reproductive outcomes and overall well-being.
